Table of Contents
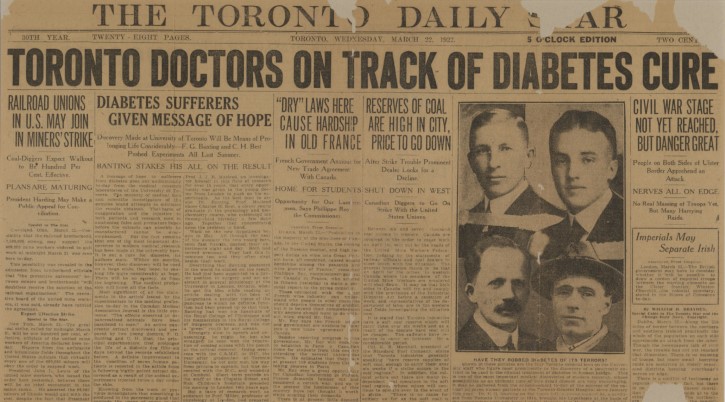
A Turning Point in Diabetes Treatment
The discovery of insulin in 1921 marked a turning point in the treatment of diabetes, transforming a once-fatal disease into a manageable condition. Before its introduction, the only available treatment was a starvation diet, which aimed to slow the progression of the disease but left patients frail and malnourished. Many children suffering from Type 1 diabetes were admitted to hospital wards, where they would inevitably succumb to diabetic ketoacidosis (DKA). The symptoms were devastating—severe dehydration, uncontrollable thirst, and eventual coma. Physicians had no means of regulating blood sugar, and patients faced an agonizing decline. With no alternative therapies, diabetes remained one of the most feared diagnoses of the time.
When insulin became available for medical use, it revolutionized diabetes care by providing a direct method to control blood sugar. The first human trial in January 1922 involved 14-year-old Leonard Thompson, who was in critical condition at Toronto General Hospital. His initial injections, though impure, produced limited results, but after refining the formula, his condition dramatically improved. Soon after, insulin became widely available, offering newfound hope to patients who had previously faced certain death. Entire hospital wards, once filled with dying children, were transformed into places of recovery and optimism. Over time, pharmaceutical companies improved insulin production, ensuring its accessibility to those in need. .
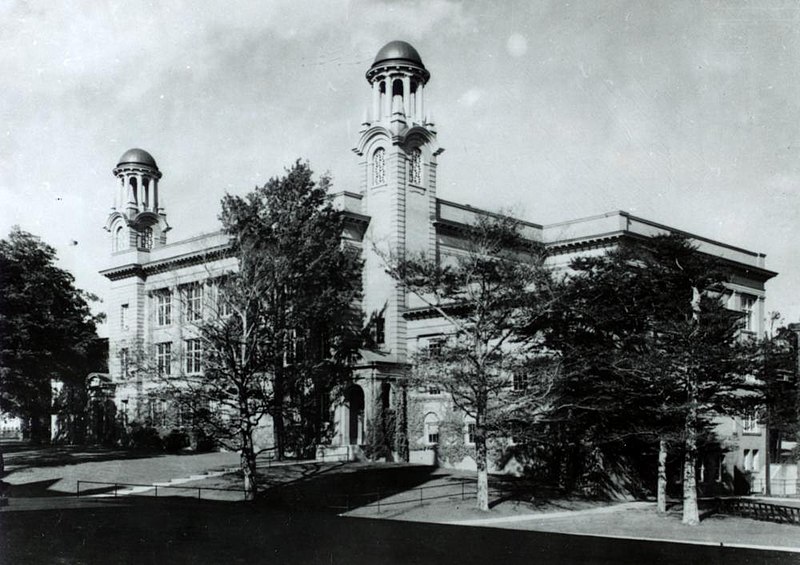
The University of Toronto and the Path to Insulin
The discovery of insulin in 1921 began with Dr. Frederick Banting’s determination to unlock the secrets of the pancreas. Inspired by previous research, he hypothesized that a specific secretion from the pancreas controlled blood sugar, but prior attempts to extract it had failed due to interference from digestive enzymes. Believing he could isolate this substance, Banting sought the support of Professor John Macleod at the University of Toronto. Although initially skeptical, Macleod provided Banting with essential resources, including a laboratory and a research assistant, Charles Best. With these tools in place, Banting and Best launched a series of groundbreaking experiments that would ultimately lead to one of the most significant medical discoveries in history.
Banting and Best’s experiments involved surgically removing the pancreas from dogs, inducing severe diabetes, and then injecting pancreatic extracts to observe their effects. Their early trials were crude, but they soon realized that ligating the pancreatic duct caused the digestive enzymes to degenerate while preserving the insulin-producing islets of Langerhans. This technique allowed them to successfully extract an active substance that significantly lowered blood sugar levels when injected into diabetic dogs. Encouraged by their results, they refined their methods and prepared for human trials. The discovery of insulin was now within reach, but further challenges, including the need for purification and large-scale production, lay ahead.
Experimental Success: The Isolation of Insulin
The discovery of insulin in 1921 was the result of months of meticulous experimentation by Frederick Banting and Charles Best. In May of that year, they began removing the pancreases of dogs, inducing diabetes and confirming the organ’s crucial role in glucose metabolism. Without insulin, the dogs exhibited extreme weight loss, excessive thirst, and dangerously high blood sugar levels. Determined to isolate the life-saving hormone, Banting devised a method to prevent the destruction of insulin-producing cells by ligating the pancreatic duct. This process allowed the exocrine tissue to degenerate while preserving the endocrine islets of Langerhans. Through this innovative approach, they successfully extracted a substance capable of regulating blood sugar levels.
The team tested a pancreatic extract on diabetic dogs, leading to immediate and remarkable results as the dogs’ blood sugar levels dropped significantly and symptoms like excessive urination and dehydration reversed. This discovery of insulin confirmed that diabetes could be managed through hormone replacement therapy, providing hope to many patients. However, challenges in refining the extract for human use remained, prompting the team to enlist biochemist James Collip to stabilize the extract for upcoming human trials.
The Role of John Macleod and James Collip
The discovery of insulin was groundbreaking, but early extracts produced by Banting and Best were inconsistent and impure, making them unsuitable for human treatment. Recognizing the need for refinement, John Macleod recruited biochemist James Collip to stabilize the extract. Collip’s expertise in protein chemistry allowed him to develop a process to purify insulin, removing harmful contaminants and ensuring consistent potency. This breakthrough was critical, as an unstable extract could cause severe side effects or fail to control blood sugar effectively. With Collip’s contributions, the team was able to produce a reliable, safe form of insulin, bringing them closer to a viable treatment for diabetic patients in urgent need.
Despite their shared goal, tensions grew within the research team. Banting, fiercely protective of his work, felt that Macleod received too much credit and resented Collip’s pivotal role in insulin purification. The strain became so intense that at one point, Banting reportedly threatened to punch Collip. However, the conflicts did not overshadow the progress made. The discovery of insulin was no longer just a laboratory breakthrough; it was ready to be tested on human patients. With a purified and stable form now available, the team prepared for their first clinical trials, which would forever change the fate of those suffering from diabetes.
The First Human Trials: A Medical Miracle
The first successful human trial of insulin in January 1922 marked a historic moment in medical science. Fourteen-year-old Leonard Thompson was in critical condition at Toronto General Hospital, suffering from severe diabetes that had left him weak and skeletal. Without treatment, he was expected to succumb to diabetic ketoacidosis within days. When doctors administered the first insulin injection, the results were disappointing due to impurities in the extract, which caused an allergic reaction. Determined to succeed, the research team, led by Frederick Banting and James Collip, worked urgently to refine the formula. Within days, they produced a purer version of insulin, giving Thompson a second chance at survival.
The refined insulin injection had an immediate and dramatic effect. Thompson’s blood sugar levels dropped to near-normal ranges, his condition stabilized, and he began to regain strength. The once-hopeless teenager, moments from death, now had a future. This success proved that insulin could effectively manage diabetes, bringing newfound hope to millions worldwide. News of the breakthrough spread quickly, and the medical community recognized its profound significance. Hospitals that had once been filled with dying diabetic children were now places of recovery. The success of Thompson’s treatment set the stage for mass insulin production, ensuring that the life-saving therapy would become widely available to those in need.
Widespread Impact: Insulin Becomes a Lifesaving Therapy
The discovery of insulin in 1921 quickly transformed from a laboratory breakthrough to a lifesaving medical treatment. With Leonard Thompson’s successful treatment proving its effectiveness, the demand for insulin skyrocketed. Pharmaceutical companies, including Eli Lilly in the United States and Connaught Laboratories in Canada, partnered with researchers to refine production methods and ensure a steady supply. By late 1922, insulin was being distributed to hospitals across North America, offering a new lease on life to diabetic patients who had previously faced an inevitable decline. No longer confined to starvation diets or awaiting a slow death, individuals with diabetes could now manage their condition and regain their strength and vitality.
As insulin became widely available, its impact was felt on a global scale. Hospital wards once filled with dying diabetic children were transformed into centers of recovery and hope. Patients who had been reduced to skeletal frames due to extreme weight loss were now gaining strength and returning to their daily lives. The discovery of insulin did not cure diabetes, but it allowed individuals to live full and productive lives despite their condition. Over the years, advances in insulin formulation and administration further improved treatment, paving the way for future innovations that continue to enhance diabetes care and management worldwide.

The 1923 Nobel Prize Controversy
The 1923 Nobel Prize in Physiology or Medicine was awarded to Frederick Banting and John Macleod for developing insulin, but it sparked controversy as Banting believed his research partner, Charles Best, deserved recognition over Macleod. Banting argued that he and Best performed the crucial experiments to isolate insulin, leading him to share his prize money with Best as a protest. In turn, Macleod divided his share with James Collip, who played a key role in purifying insulin for human use.
Despite the dispute, the Nobel Prize cemented the significance of the team’s discovery and its impact on diabetes treatment worldwide. The controversy underscored the complexities of scientific collaboration, where multiple contributors played essential roles, but only some received formal recognition. Though Banting and Best are often credited as the primary discoverers, Macleod’s leadership and Collip’s purification techniques were essential in turning insulin into a viable medical treatment. Regardless of their disagreements, their collective efforts saved millions of lives. The Nobel Prize, even amid controversy, acknowledged the discovery of insulin as a historic achievement that transformed medicine and gave those with diabetes a chance at a longer, healthier life.
Transforming Diabetes Treatment: A Global Shift
With the widespread availability of insulin, diabetes treatment evolved from a desperate struggle for survival into a manageable medical condition. Previously, patients were subjected to extreme starvation diets, drastically reducing carbohydrate intake in an attempt to slow disease progression. These diets left individuals malnourished and weakened, often delaying death rather than preventing it. The introduction of insulin allowed patients to regulate their blood sugar through regular injections, restoring their strength and improving their quality of life. For the first time, diabetes was no longer an immediate death sentence but a condition that could be controlled. Hospitals transformed from places of hopelessness into centers of recovery, where patients could regain their health and resume normal lives.
Beyond its immediate impact, the discovery of insulin revolutionized the field of endocrinology, paving the way for deeper understanding of hormone regulation. Researchers began exploring ways to improve insulin formulations, leading to longer-acting variants and more efficient delivery systems. Over the decades, advancements such as insulin pumps, synthetic human insulin, and continuous glucose monitoring reshaped diabetes care. Scientists also expanded their research into other endocrine disorders, applying lessons learned from insulin therapy to develop treatments for thyroid, adrenal, and growth hormone deficiencies. Today, diabetes management continues to evolve, with ongoing research exploring potential cures through gene therapy and beta-cell transplantation, demonstrating the lasting legacy of insulin in medical science.
The Role of Pharmaceutical Companies in Insulin Production
As the demand for insulin surged following its discovery, pharmaceutical companies stepped in to refine production and ensure widespread availability. Eli Lilly, in collaboration with the University of Toronto, became the first company to mass-produce insulin, standardizing its formulation and making it accessible to patients across North America. This partnership was instrumental in transforming insulin from an experimental treatment into a reliable, lifesaving therapy. Soon after, other pharmaceutical companies joined the effort, scaling up production and improving purification techniques. Their involvement not only ensured a steady supply of insulin but also contributed to advancements in its formulation, leading to more effective and longer-lasting options for diabetes management.
In the decades that followed, insulin production continued to evolve. The introduction of synthetic human insulin in the 1980s was a major breakthrough, as it reduced allergic reactions associated with earlier animal-derived insulin. This innovation was followed by the development of insulin analogs in the 21st century, which provided even greater precision in blood sugar control. These advancements allowed for more flexible dosing schedules, better mimicking the body’s natural insulin response. Today, ongoing research focuses on even more sophisticated delivery methods, such as smart insulin pens and implantable insulin devices, ensuring that the legacy of pharmaceutical involvement in insulin production continues to improve the lives of people with diabetes.

Banting’s Legacy: A Life Dedicated to Medicine
Frederick Banting’s contributions to medicine extended far beyond the discovery of insulin. Despite the tensions surrounding his work, he remained dedicated to scientific research, particularly in the fields of physiology and military medicine. During World War II, Banting focused on developing treatments for aviation-related health issues, including the effects of high-altitude flight on pilots. His research aimed to improve pilot endurance and safety, highlighting his commitment to advancing medicine beyond diabetes treatment. Tragically, his life was cut short when his plane crashed in Newfoundland in 1941 during a wartime mission. Though he died at just 49, his impact on medical science was already cemented in history.
Banting’s legacy continues to be honored worldwide. His role in the discovery of insulin transformed diabetes from a fatal disease into a manageable condition, saving millions of lives. Today, numerous institutions, research centers, and awards bear his name, ensuring that his contributions are never forgotten. The Banting Medal for Scientific Achievement remains one of the highest honors in diabetes research, awarded to those who continue advancing treatment and understanding of the disease. His birthday, November 14, is recognized globally as World Diabetes Day, serving as a reminder of his invaluable work. Through his discoveries, Banting’s influence endures, shaping the future of medical science and patient care.
The Evolution of Diabetes Treatment Since 1922
Since the discovery of insulin in 1921, diabetes treatment has progressed far beyond daily injections. One of the most significant innovations is the development of continuous glucose monitors (CGMs), which provide real-time blood sugar readings without the need for constant finger pricks. These devices help patients maintain tighter glucose control, reducing the risk of complications. Insulin pumps have also revolutionized treatment by delivering precise doses of insulin throughout the day, mimicking the pancreas’s natural function more closely. More recently, artificial pancreas technology has emerged, combining CGMs and insulin pumps with algorithms that automatically adjust insulin delivery. These advancements have greatly improved the quality of life for people living with diabetes.
While insulin therapy remains the primary treatment, researchers are actively exploring potential cures. Gene therapy is being studied as a way to reprogram cells to produce insulin naturally, eliminating the need for injections altogether. Beta-cell transplantation, which involves implanting insulin-producing cells from donors, has shown promising results in restoring blood sugar control. However, challenges such as immune system rejection and limited donor availability still need to be overcome. Despite these hurdles, the future of diabetes treatment continues to evolve rapidly. With ongoing research and technological innovation, scientists remain committed to finding more effective and sustainable solutions, offering hope for a world where diabetes can be cured.
The Enduring Impact of Insulin on Medicine and Humanity
The discovery of insulin remains one of the most significant breakthroughs in medical history. It transformed diabetes from a fatal disease into a manageable condition, saving countless lives. The legacy of Banting, Best, Macleod, and Collip is not just in their discovery, but in the hope and opportunity they gave to millions of people. Insulin’s impact extends beyond diabetes—it paved the way for hormone replacement therapies and advances in biotechnology. Over a century later, their work continues to inspire medical innovation, proving that scientific perseverance can lead to life-changing discoveries.
How useful was this post?
Click on a star to rate it!
Average rating / 5. Vote count:
No votes so far! Be the first to rate this post.
Author
-
Meet Dr. Kendall Gregory, a highly accomplished professional with a remarkable academic background and a deep passion for empowering individuals through knowledge. Dr. Gregory’s educational journey began with a Bachelor of Science degree, followed by a Doctor of Chiropractic Medicine, focusing on diagnosing and treating musculoskeletal conditions. He further expanded his expertise with a Master's degree in Oriental Medicine, specializing in acupuncture and Chinese herbology, and a Master's degree in Health Care Administration, emphasizing his dedication to improving healthcare systems. Dr. Gregory combines his extensive knowledge and practical experience to provide comprehensive and integrative healthcare solutions. Through his writings, he aims to inspire individuals to take charge of their health and make informed decisions.
View all posts